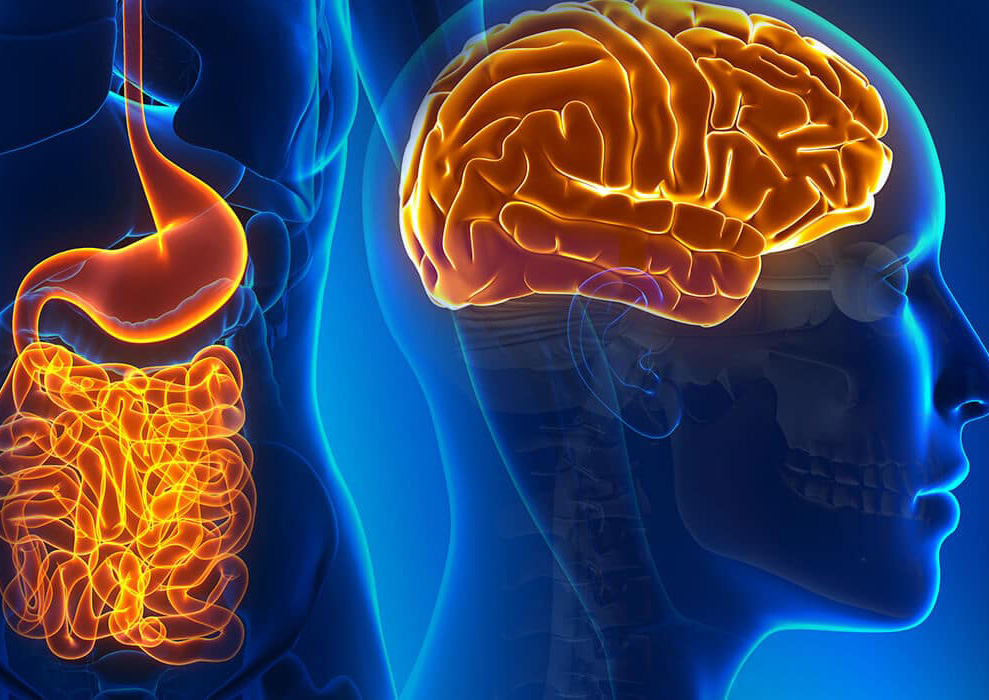
The Link Between Gut Health and Your Brain
The connection between the gut microbiome and brain function represents an incredibly exciting, emerging area of research. Diet is a major, modifiable factor that can dramatically affect the gut microbiome, which in turn influences mental health. Here, we explain the gut-brain connection, and the role of the diet in supporting both gut and mental health.
The gut microbiome
The gut microbiome is made up of up to 100 trillion microorganisms, primarily bacteria, within the gut. We each have a microbiome unique to us – a bit like fingerprints. As a result, there is no standard definition of a ‘healthy’ microbiome, however, below are some key features:
– Microbial richness (total number of microbes)
– Microbial diversity (number of different microbes – ideally striking a balance between ‘good’ and ‘bad’ bacteria)
– Microbial resistance (the microbiome’s ability to resist disruption)
– Microbial resilience (the microbiome’s ability to return to a healthy state after disruption)
Within the gut, bacteria obtain energy from undigested food. As a result, specific nutrients and dietary patterns can shape our gut microbiome. When we eat different foods, we produce different bacteria by-products. These influence various bodily functions, including brain health and mood. This demonstrates the clear link between diet, our microbiome and our brain.
The gut-brain axis
The connection between the gut microbiome and brain, referred to as the gut-brain-axis- is bi-directional. This means that the brain influences the gut and the gut influences the brain. It’s this connection that is responsible for ‘gut feelings’ and sensations of ‘butterflies’ when feeling nervous or excited. The precise mechanisms underlying the gut-brain axis remain unknown. However, it is known that neural (brain), endocrine (hormonal) and immune pathways are involved.
These pathways include:
– The vagus nerve: communicates signals between the brain and other organs, which regulate digestion, heart rate and respiratory rate.
– The immune system: The gut microbiome regulates immune responses throughout the body. Wide-spread low-grade inflammation is the result of an immune response. This often coincides with a range of neurological conditions, including autism spectrum disorders, Alzheimer’s disease and Parkinson’s disease.
– The neuroendocrine system (I.e. brain/hormone system), including the hypothalamic-pituitary-adrenal (HPA) axis. Recent research has highlighted the ability of the gut microbiome to activate (‘switch on’) the HPA axis, which is involved in stress responses, mood and emotional regulation.
– Neurotransmitters (chemical messengers). Current research suggests that the gut microbiota influences the production and metabolism of multiple neurotransmitters (carry messages around the body), including:
o Serotonin (the happy hormone) – involved in mood, sleep, cognition, and appetite regulation.
o Dopamine (the reward chemical) – associated with reward-motivated behaviour and found to be affected by gut microbiome.
– Metabolites such as short-chain fatty acids (SCFAs). We produce SCFAs after eating carbohydrate-containing foods such as legumes and wholegrains. SCFAs support memory, cognition, mood, stress responses and metabolism. They are shown to reduce risk of conditions such as Alzheimer’s disease.
Diet and the gut microbiome
Diet significantly influences the composition and diversity of the gut microbiome.
An anti-inflammatory Mediterranean dietary pattern, is associated with a more diverse microbiome. The Mediterranean diet is rich in plant foods including vegetables, fruits, legumes, nuts, and seeds. It features more seafood in place of red meat, and includes mostly unsaturated (‘healthy’) fats such as extra virgin olive oil, avocado and oily fish.
The following dietary inclusions have all been associated with a healthy gut microbiome:
– Plant foods (fruit, veggies, herbs, spices, nuts, seeds, legumes, wholegrains)
– Healthy fats (nuts, seeds, avocado, oily fish, extra virgin olive oil)
– Polyphenols (found in herbs, spices, colourful fruit and veg, red wine, dark chocolate and tea)
– Fermented foods (kefir, sauerkraut, miso, kimchi, kombucha, tempeh)
Meanwhile, the traditional Western diet is shown to negatively impact the gut microbiome. It is typically made up of large amounts of saturated fat, animal protein and refined carbohydrates. Research indicates that the following foods, in excess, negatively affect the gut microbiome:
– Meat, particularly red and processed meat
– Saturated fat (fatty meat, coconut oil/cream/yoghurt, cream, butter, chocolate, baked good, fried foods etc)
– Foods high in added sugar (baked goods, lollies, ice-cream, soft drinks, chocolate)
– Artificial sweeteners (the jury is still out on their impact on the gut microbiome, but given we don’t know about their long-term impact and safety, it makes sense to limit them)
Find our top 12 foods for optimal mental health here
For expert, personalised dietary advice for optimal mental health, book your first appointment with one of our wonderful accredited practising dietitians today.
Written by Caitlin Branch, Student Nutritionist, and Amanda Smith, Accredited Practicing Dietitian.
References
Bear, T. L. K., Dalziel, J. E., Coad, J., Roy, N. C., Butts, C. A., & Gopal, P. K. (2020). The role of the gut microbiota in dietary interventions for depression and anxiety. Advances in Nutrition, 11(4), 890-907. https://doi.org/10.1093/advances/nmaa016
Berding, K., Vlckova, K., Marx, W., Schellekens, H., Stanton, C., Clarke, G., Jacka, F., Dinan, T. G., & Cryan, J. F. (2021). Diet and the microbiota-gut-brain axis: Sowing the seeds of good mental health. Advances in Nutrition,12(4), 1239-1285. https://doi.org/10.1093/advances/nmaa181
Chakrabarti, A., Geurts, L., Hoyles, L., Iozzo, P., Kraneveld, A. D., La Fata, G., Miani, M., Patterson, E., Pot, B., Shortt, C., & Vauzour, D. (2022). The microbiota-gut-brain axis: Pathways to better brain health. Perspectives on what we know, what we need to investigate and how to put knowledge into practice. Cellular and Molecular Life Sciences, 79(2), 1-15. https://doi.org/10.1007/s00018-021-04060-w
Gropper, S. S., Smith, J. L., & Carr, T. P. (2022). Advanced nutrition and human metabolism (8th ed.). Cengage.
Mörkl, S., Butler, M. I., Holl, A., Cryan, J. F., & Dinan, T. G. (2020). Probiotics and the microbiota-gut-brain axis: Focus on psychiatry. Current Nutrition Reports, 9(3), 171-182. https://doi.org/10.1007/s13668-020-